1801006064 LONG CASE
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 50 year old man who is a worker in an ice factory and resident of Miryalguda came with chief complaints of weakness of right upper limb and lower limb , slurring of speech and deviation of mouth to left side since 5 days (12/03/2023)
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 1 month back.
Then he developed weakness of left upper limb and lower for which he went to the local hospital and the symptoms resolved in 3 days.There he was also diagnosed with hypertension for which he took medication for 20 days and stopped since 10 days.
Now again on 12/03/2023 at morning 4 am he developed weakness of right upper limb and lower limb .He also developed slurring of speech and deviation of mouth towards left.Again he was taken to local hospital and CT scan was done and they referred to our hospital.They came to our hospital on 13/03/2023
No history of vomiting headache giddiness, altered sensorium,neck stiffness, abnormal movements, behavioural abnormalities
PAST HISTORY
History of fracture to right elbow 30 years ago.
No history of diabetes, Asthma, tuberculosis, epilepsy, chronic kidney disease
No history of trauma to head
No history of any surgeries
PERSONAL HISTORY
Diet Mixed
Appetite Normal
Sleep Adequate
Bowel and bladder Regular
Addictions Alcoholic since 20 yrs and chews Gutka
DAILY ROUTINE
Before the incident he used to get up around 4am goes for work and come by 9 am and have breakfast and again goes back for work and come back by around 1 pm for lunch and goes back to work and come back home at 9 pm then he will have his dinner and sleep around 10 pm
After the incident
He went for work for 20 days and then stopped doing the work.His strength to do works is decreased
FAMILY HISTORY
No significant family history
TREATMENT HISTORY
Took medication for hypertension (Atenolol and Amlodipine) for 20 days and stopped since 10 days
GENERAL EXAMINATION
Patient is conscious coherent and cooperative
Moderately built and nourished
Pallor Absent
Icterus Absent
Cyanosis Absent
Clubbing Absent
Generalised lymphadenopathy Absent
Edema Absent
Vitals
Temperature Afebrile
Pulse pressure 75 beats per min
Blood pressure 130/70 mm Hg
Respiratory rate 17 cycles per min
GRBS 109mg/dl
SYSTEMIC EXAMINATION
CENTRAL NERVOUS SYSTEM
Dominance -Right handed
Higher mental functions
Conscious
Oriented to time place and person
Memory -Immediate, recent and remote
Slurring of speech
Cranial nerve examination
I- Olfactory nerve- sense of smell Normal
II- Optic nerve-
Visual acuity
Field of vision. Normal
Colour vision normal
III, IV, VI. Rt lft .
EOM. N. N
diplopia. Absent. Absent
nystagmus absent. Absent
ptosis. Absent. Absent
Direct and indirect
Light reflex present
V- Masseter, temporalis and pterygoid muscles are normal on both sides.
Corneal reflex, conjunctival reflex present on both sides
VII- - Deviation of mouth to left Upper half of right side and left side of face is normal
Sensory Taste over any.2/3 rd of tongue present
VIII- no hearing loss ,no vertigo
IX- no difficulty in swallowing
X- Vagus nerve -No difficulty in swallowing
XI -sternocleidomastoid contraction present,
Trapeziu- shrugging of shoulders against resistance present
XII - No deviation of tongue,tongue movements normal ,no fasciculations
Motor system
Tone Right. Left
Upper limb Increased. Normal
Lower limb Increased Normal power. Right. Left
Upper limb 3/5 4/5
Lower limb 3/5 4/5
Superficial reflxes
Corneal reflex normal on both sides
Conjunctival reflex normal on both sides
Plantar reflex Muted on right side
https://youtube.com/shorts/zBZt8oAn2pI?feature=share
Deep tendon reflexes Right Left
Biceps +++ ++
Triceps. +++ ++
Supinator +++ ++
Knee. Jerk +++ ++
Ankle jerk +++ ++
Sensory system
Spinothalamic. Rt. Lft
Crude touch + +.
Pain + +
Temperature + +
Posterior column
Fine touch + +
Vibration Normal
Cortical
Two point discrimination- able to discriminate
Tactile localization -able to localise
Cerebellar Examination
Finger nose test-Normal
Heel shin test -Normal
Finger finger nose test -Normal
No Dysdiadochokinesia
No meningeal signs
Examination of spine-Normal
Gait
Deep tendon reflexes Right side
Biceps
https://youtube.com/shorts/Len1bmONhxo?feature=share
Triceps
https://youtube.com/shorts/71yp3BvJ84s?feature=share
Knee jerk
https://youtube.com/shorts/x59TzodyNRc?feature=share
Ankle jerk
Supinator
Cerebellar functions
https://youtube.com/shorts/QMVnw82LWYY?feature=share
RESPIRATORY SYSTEM
CARDIOVASCULAR SYSTEM
Inspection :
Shape of chest- elliptical shaped chest
No engorged veins, scars, visible pulsations
JVP is not raised
Palpation :
Apex beat can be palpable in 5th inter costal space medial to mid clavicular line
No thrills and parasternal heaves can be felt
Auscultation :
S1,S2 are heard
no murmurs
ABDOMINAL EXAMINATION
Inspection -
Umbilicus - inverted
All quadrants moving equally with respiration
No scars, sinuses and engorged veins , visible. pulsations.
Hernial orifices- free.
Palpation -
soft, non-tender
no palpable spleen and liver
Percussion:Resonant note heard
Auscultation- normal bowel sounds heard
PROVISIONAL DIAGNOSIS
Cerebrovascular accident with Right hemiparesis .
INVESTIGATIONS
Anti HCV antibodies rapid - non reactive
HIV 1/2 rapid test - non reactive
Random Blood sugar - 109 mg/dl
Fasting blood sugar - 114 mg/dl
Hemoglobin- 13.4 gm/dl
WBC-7,800 cells/mm3
Neutrophils- 70%
Lymphocytes- 21%
Eosinophils- 01%
Monocytes- 8%
Basophils- 0
PCV- 40 vol%
MCV- 89.9 fl
MCH- 30.1 pg
MCHC- 33.5%
RBC count- 4.45 millions/mm3
Platelet counts- 3.01 lakhs/ cu mm
Peripheral Smear
RBC - normocytic normochromic
WBC - with in normal limits
Platelets - Adequate
Complete Urine Examination
Colour - pale yellow
Appearance- clear
Reaction - acidic
Sp.gravity - 1.010
Albumin - trace
Sugar - nil
Bile salts - nil
Bile pigments - nil
Pus cells - 3-4 /HPF
Epithelial cells - 2-3/HPF
RBC s - nil
Crystals - nil
Casts - nil
Amorphous deposits - absent
Liver Function tests
Total bilirubin - 1.71 mg/dl
Direct bilirubin- 0.48 mg/dl
AST - 15 IU/L
ALT - 14 IU/L
Alkaline phosphatase - 149 IU/L
Total proteins - 6.3 g/dl
Albumin - 3.6 g/dl
A/G ratio - 1.36
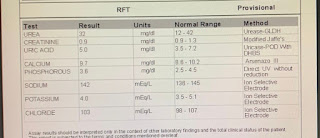
Blood urea - 19 mg/dl
Serum creatinine - 1.1 mg/dl
Electrolytes
Sodium - 141 mEq/L
Potassium - 3.7 mEq/L
Chloride - 104 mEq/L
Calcium ionised - 1.02 mmol/L
ECG

















Comments
Post a Comment